The time to talk with our loved ones is now, in the living years
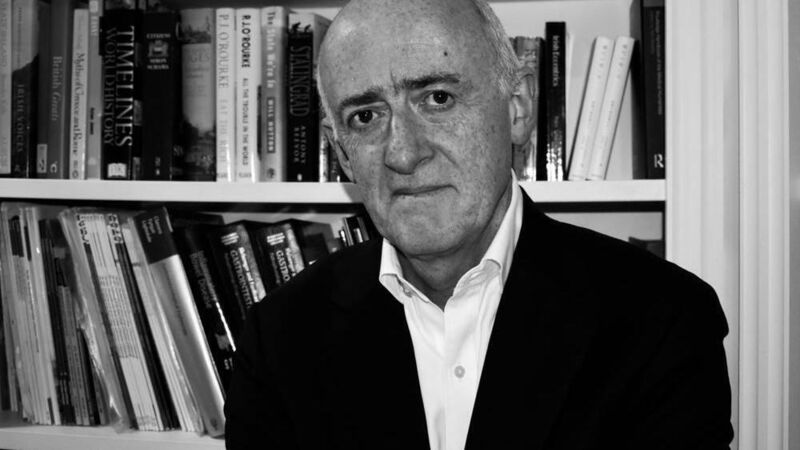
Dr Seamus O'Mahony highlights a recent survey which shows the profound regret many bereaved people suffer for not having had meaningful conversations with their loved ones.
The Irish, it is said, are great with the dead, but not so good with the dying.
A new survey carried out by the insurer Royal London would seem to bear this out. One thousand adults were asked about their experience with death, dying, and bereavement.













