Stroke Awareness Week: Speedy and appropriate treatment in hospital is key to recovery
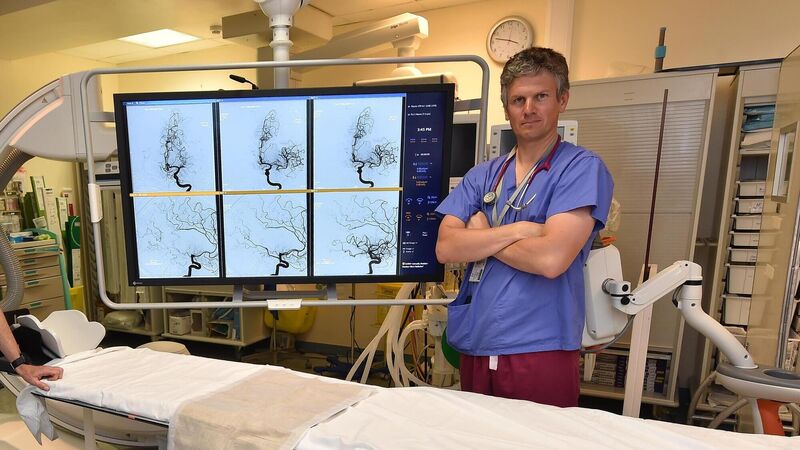
Dr Liam Healy, clinical lead for stroke services, pictured in the thrombectomy suite at the Cork University Hospital. Picture Dan Linehan
There are many initiatives aimed at diverting patients away from overstretched emergency departments — but these never apply to people with symptoms of stroke, says Liam Healy, consultant stroke physician at Cork University Hospital, who oversees the country’s busiest inpatient stroke service.
In the case of stroke, speed is of the essence, he warns. “If someone presents with stroke-like symptoms, they can be expected to be seen as quickly as possible. Stroke patients are a priority, along with other serious presentations at the emergency department.”











