Stroke Awareness Week: Stroke procedure can help bring patients back to normal living
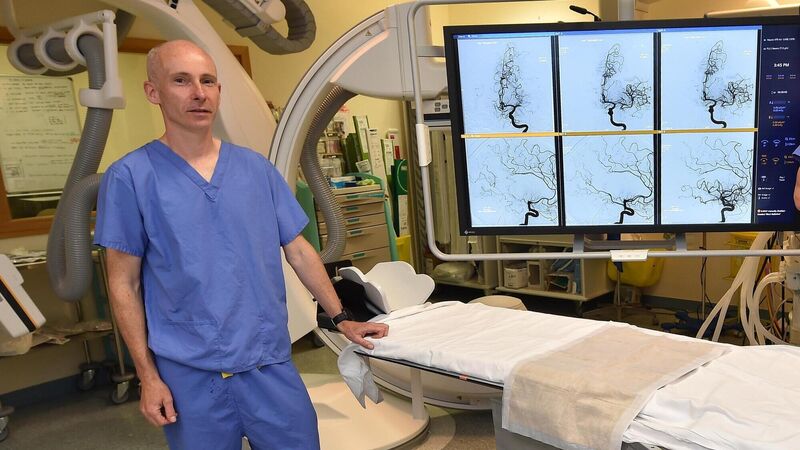
Dr Noel Fanning consultant neuroradiologist in the thrombectomy suite at the Cork University Hospital. Picture Dan Linehan
With huge advances in the treatment of stroke over the last two decades, there is now the possibility of reversing the effects of some of the most severe strokes, bringing patients back to normal living.
This is where thrombectomy comes into the picture, says Dr Noel Fanning, consultant neuroradiologist at the Cork University Hospital (CUH) stroke unit.











