Take it from me: Four female doctors on their menopause experience
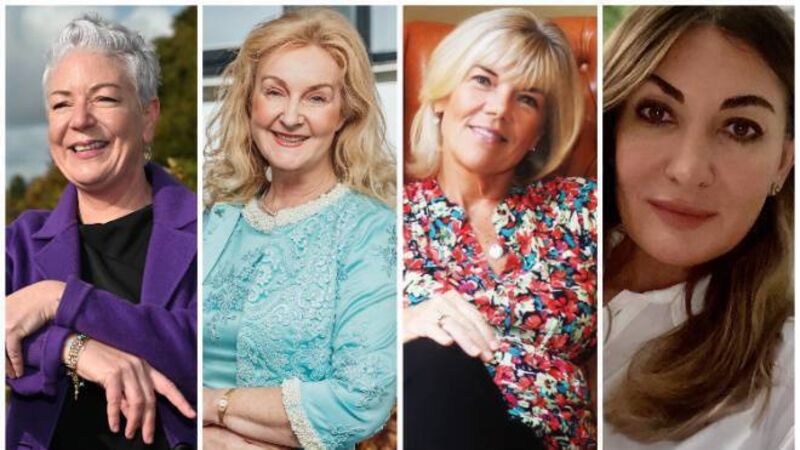
Some of the medics that have discussed their menopause experience with Helen O'Callaghan.
Try from €1.50 / week
SUBSCRIBE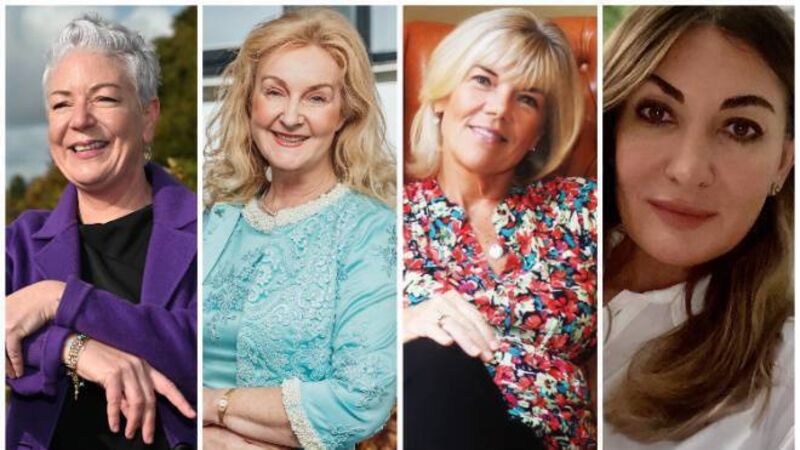
Some of the medics that have discussed their menopause experience with Helen O'Callaghan.
Menopause is a key transition — and every woman will undergo it. Yet it has not always been talked about openly.
Here, we talk to four doctors about navigating their own perimenopause/menopause. We asked each a range of questions: About when they first noticed signs of a hormone shift, about symptoms and how these affected their lives. What steps did they take to manage symptoms? Was HRT part of their solution? How important was family/friend support — and if they have an ongoing self-care plan?
Already a subscriber? Sign in
You have reached your article limit.
Annual €130 €80
Best value
Monthly €12€6 / month
Introductory offers for new customers. Annual billed once for first year. Renews at €130. Monthly initial discount (first 3 months) billed monthly, then €12 a month. Ts&Cs apply.
CONNECT WITH US TODAY
Be the first to know the latest news and updates
Newsletter
The best food, health, entertainment and lifestyle content from the Irish Examiner, direct to your inbox.
Newsletter
The best food, health, entertainment and lifestyle content from the Irish Examiner, direct to your inbox.

Our team of experts are on hand to offer advice and answer your questions here
© Examiner Echo Group Limited