Our son's life could have been saved if doctors were sepsis aware
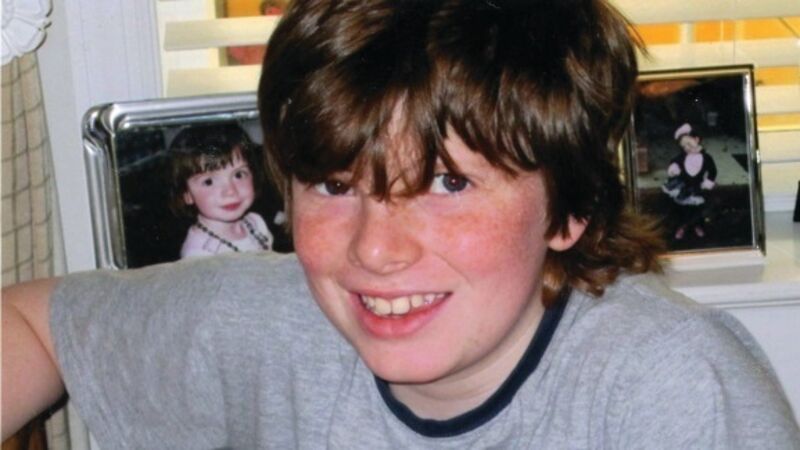
Ciaran Staunton’s son was 12 when he cut his elbow during a basketball game. When he became ill overnight, his mother, Orlaith, from Drogheda Co Louth, brought him to a paediatrician in New York where he exhibited low blood pressure, pain, fever and mottled skin.
The paediatrician diagnosed a stomach bug and a second doctor at an emergency department later agreed with this original diagnosis. The second doctor took blood tests for other infections but didn’t check them before discharging Rory.










