Positive progress for women with endometriosis
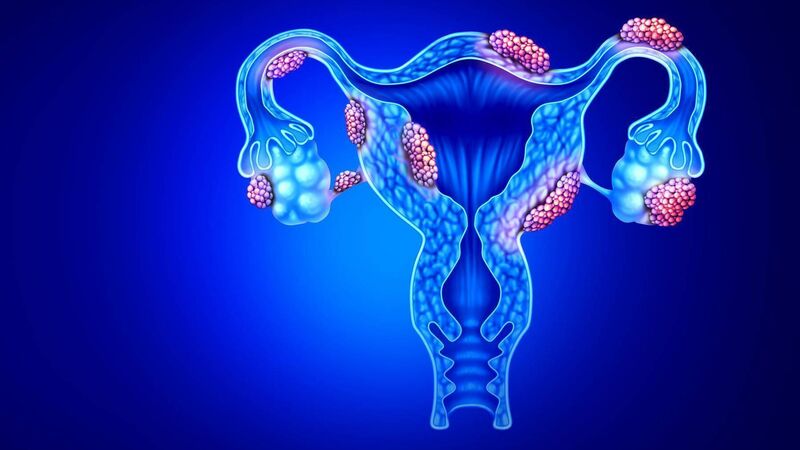
Endometriosis occurs when endometrial-like tissue locates beyond the uterus, causing a cascade effect. The abnormal tissue secretes substances that irritate surrounding tissues, causing them to bleed
Try from €1.50 / week
SUBSCRIBE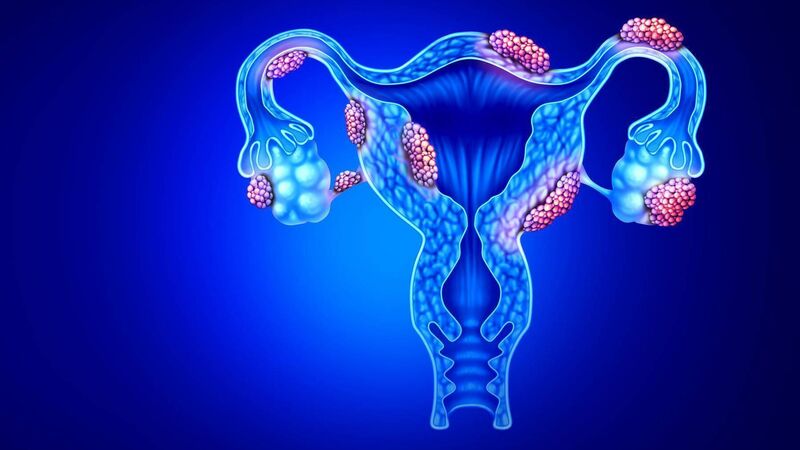
Endometriosis occurs when endometrial-like tissue locates beyond the uterus, causing a cascade effect. The abnormal tissue secretes substances that irritate surrounding tissues, causing them to bleed
‘HOPE’, ‘Possibility’, ‘Excitement’ — increasingly this year, these positive words have been used in the same sentence as endometriosis, a common gynaecological condition affecting one in ten women.
In March, University of Oxford researchers collaborating with teams worldwide published the largest-ever study of the genetic basis of endometriosis.
Already a subscriber? Sign in
You have reached your article limit.
Annual €130 €80
Best value
Monthly €12€6 / month
Introductory offers for new customers. Annual billed once for first year. Renews at €130. Monthly initial discount (first 3 months) billed monthly, then €12 a month. Ts&Cs apply.
CONNECT WITH US TODAY
Be the first to know the latest news and updates
Newsletter
The best food, health, entertainment and lifestyle content from the Irish Examiner, direct to your inbox.
Newsletter
The best food, health, entertainment and lifestyle content from the Irish Examiner, direct to your inbox.

Our team of experts are on hand to offer advice and answer your questions here
© Examiner Echo Group Limited