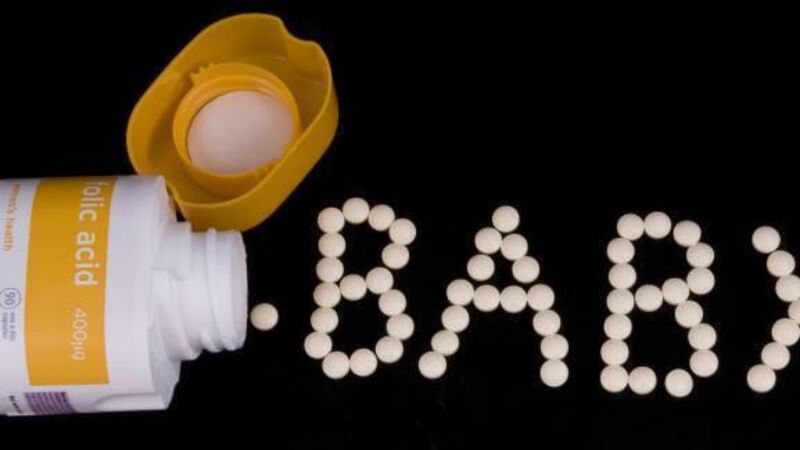
Taking your daily dose: Nutrition and Neural Tube Defects
As their name suggests, they’re caused by a failure of the foetal neural tube to close in early pregnancy, meaning that the structures which later become the child’s spinal column and skull fail to develop properly.
Spina bifida shows a spectrum of disease severity ranging from mild paralysis of the lower limbs, right through to full paralysis of all four limbs with associated bladder and bowel dysfunction. However, anencephaly, which prevents the development of structures which later house the brain, is considered a fatal condition, with most of these infants surviving less than 24 hours.











