Head games: reconsidering what we know about treating concussion
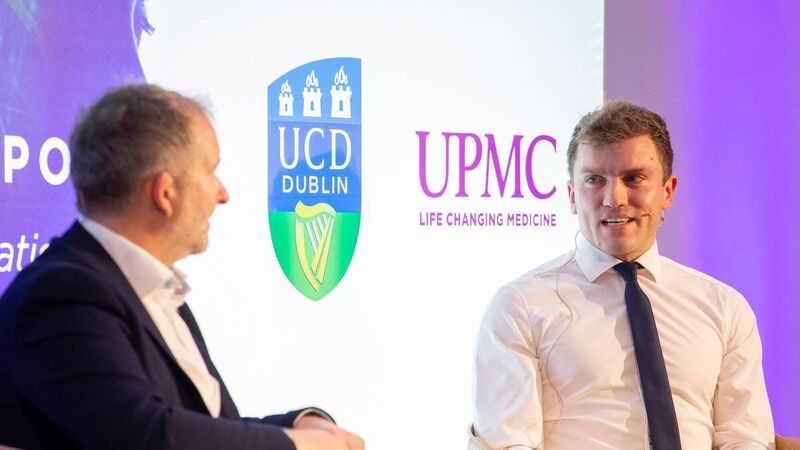
REFLECTION: All Ireland-winning hurler Shane O’Donnell speaks to Ger Gilroy at UPMC’s seminar “Concussion in Sport – A National Conversation” in UCD on Saturday.
Here’s a thought. What if most of the little we thought we knew about concussion was wrong? What if the good intentions we had, as doctors and as coaches and as parents, when telling kids and others to pull the blinds and climb into bed until the bad stuff stops was making the problem worse rather than better?
We’re all learning but the lessons come at a cost.











