Neil Michael: Under-investment in public health undermines zero Covid efforts
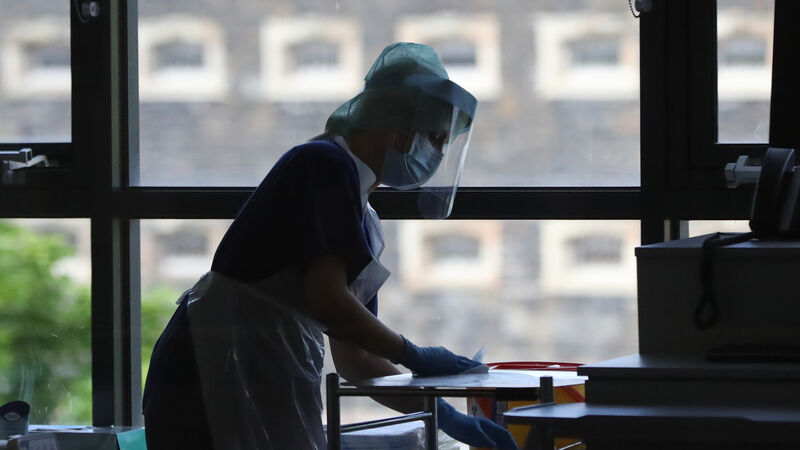
The dire state of regional public health departments - this country’s “forgotten frontline” - could hinder our efforts to attain zero covid
Professor Ivan Perry is one of an ever-widening community of academics and professionals in favour of aiming for zero or near zero-Covid.
But University College Cork's Professor of Public Health and other public health experts see a rather large elephant in the room.













