Grieving family seek changes to Irish Medical Council probes
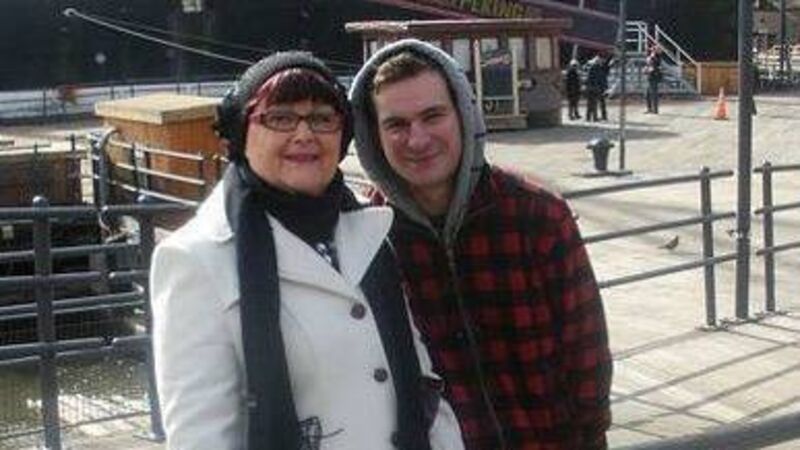
James Hyland, with his late mother Eileen Hyland. The family believes that Eileen's life may have been cut short and her suffering intensified because of alleged failures in her care.
A grieving family is calling for changes to the Irish Medical Council after a consultant who they accused of mistreating their late mother left the country when an investigation into his practice was to be launched.
Eileen Hyland, 68, was refused a potentially life-saving treatment for thyroid cancer, called radioactive iodine therapy (RAIT), in Cork University Hospital in 2016.










