Emotions run high at end of inquiry over birth of boy
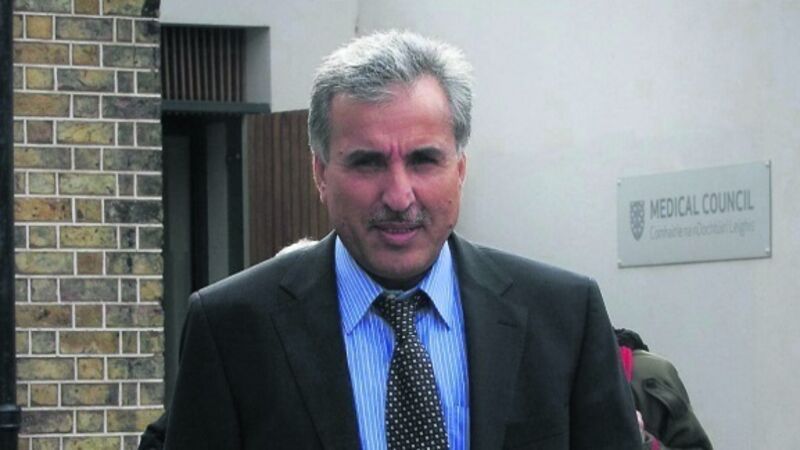
The allegations against Mohammad Ilyas Khan from Clonmel claim he did not put an adequate treatment plan in place following the birth of a baby boy at South Tipperary General Hospital on June 15, 2012, and the subsequent diagnosis of hypoxic ischaemic encephalopathy (hypoxia), or lack of oxygen to the brain.
Specifically, it is alleged that Dr Khan failed to make sufficient arrangements so the baby, now three, could receive hypothermic, or ‘cooling’, treatment.













