I froze my eggs at 34 — every woman should be given this opportunity in their early 20s

Tara Logan Buckley: “I got absolutely no education on fertility when I was young, I got nothing in school or college. I come from a clinical psychology background, where there is a lot of science. I didn’t know the number of eggs dramatically declines after 30.”
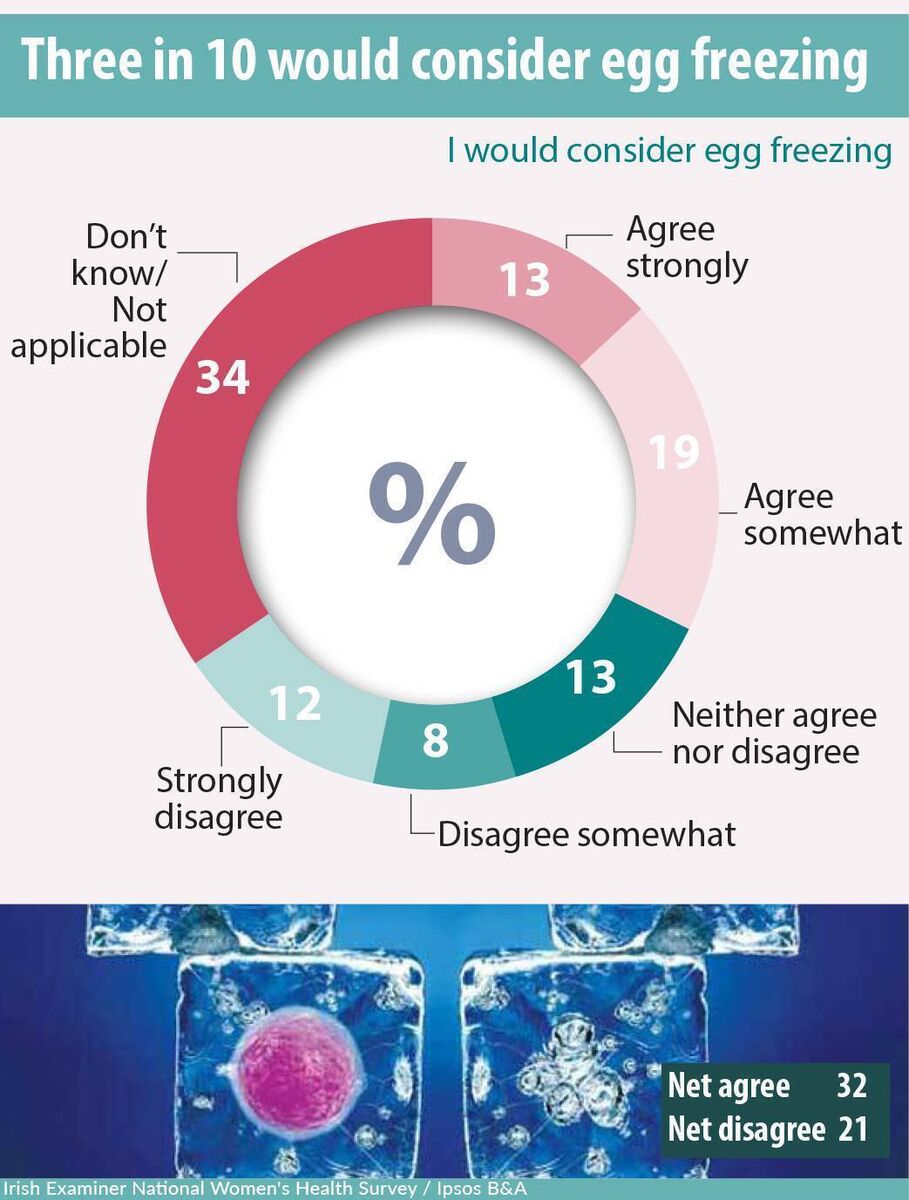
A third of women would consider freezing their eggs, they said in the Irish Examiner National Women’s Health Survey, conducted by Ipsos B&A.
Egg freezing used to be an option provided to women who, for medical reasons — such as cancer treatment or a family history of early menopause — faced risks to their fertility and to ensure the capacity to conceive.
Increasingly, the option is available to women who can afford it, who may not be in a couple, or who may not be ready to start trying for a baby, but who want to preserve the chance.
This procedure is called ‘social egg freezing’ — or the more technical term, elective oocyte cryopreservation.
According to the latest figures from the Health Products Regulatory Authority, the number of eggs frozen for future use in fertility treatments has increased almost fivefold, from 2,590 in 2019 to 12,890 in 2024.
The number of eggs a woman has drops off significantly from the age of 30. Retrieving 10-20 eggs is considered optimal, and, for some women, achieving this amount may require multiple cycles.
Health authorities and clinics caution that no number of eggs will guarantee a baby, but freezing is a way women can improve their chances, particularly if they are under the age of 35.

Lauren Murphy, a senior fertility midwife at the Thérapie Clinic in Limerick, and working for a decade in the field, says: “In the last five years or so, there’s definitely more women looking at fertility preservation and also single motherhood by choice.”
Even when people come to the clinic as part of a couple, Murphy says they would advise egg freezing in addition to embryo freezing. Where a couple freezes embryos and the relationship doesn’t work out, any frozen embryos would require the consent of the former partner for the embryos to be used. Frozen eggs are the sole ownership of the woman.
After initial consultation, the subsequent steps are assessments with scans and blood testing. The medical team uses the test results to determine the number of egg-retrieval cycles that may be necessary.
Murphy says: “There is no diagnostic test on the market to assess the quality of eggs, so, at initial testing, we’re really focusing on a test to identify the quantity. That [quantity] will also influence the drug dosages that we need to give to stimulate the ovaries.”
A blood test for AMH (anti-mullerian hormone) levels indicates a woman’s ovarian reserve or egg numbers.
Murphy says they would also recommend a trans vaginal ultrasound scan. It can be done on any cycle date and takes about 15 minutes.
The ovaries are measured, and all the individual anterior follicles (sacs containing immature eggs) are counted.
The information provides the medical team with a better understanding of how many eggs can be retrieved from a single egg-freezing cycle.
Three years ago, at the age of 34, Tara Logan Buckley decided to freeze her eggs.
She is a chartered clinical psychologist and wanted to get to a senior level in her career before motherhood.
She was in a relationship, but did not see a future and a family with that person. Housing was another factor.
She wanted to have the security of a home before starting a family: “I was living in Dublin, I had been a student for quite a long time, there were a lot of debts that needed to be repaid, and I just didn’t have my own property.
"As you know, housing market prices have dramatically increased, and they’re rising all the time. I didn’t want to be living in a house that I couldn’t afford and couldn’t give a child the quality of life they needed or give myself a quality of life and then be financially stressed.”
Outside of these social and environmental factors, Buckley was compelled by the science: “I got absolutely no education on fertility when I was young, I got nothing in school or college. I come from a clinical psychology background, where there is a lot of science. I didn’t know the number of eggs dramatically declines after 30.”
“When I started, it was more like ‘Will I, won’t I?’ When I did the research, I was like ‘Wow, this is frightening.’ Every woman should be told this, and every woman should be given the opportunity in their early 20s to do this.
“When I went to the consultant, he said to me ‘Look, you’re doing it as an insurance.’ I may choose never to have a child, unless circumstances change. There is also a silver lining to that, where another woman might use them in the future if I don’t use them, but also the fact that I could use all of them, but none of them might work.”
![Tara Logan Buckley: "You need to be prepared to be really, really regimental with your routine. Having people around you for support, as well. I felt OK until I got to those last 48 hours, where I couldn’t wait to go in and get [the eggs] out.” Tara Logan Buckley: "You need to be prepared to be really, really regimental with your routine. Having people around you for support, as well. I felt OK until I got to those last 48 hours, where I couldn’t wait to go in and get [the eggs] out.”](/cms_media/module_img/9339/4669988_16_articleinline_Tara_Logan_Buckley.jpeg)
When Logan Buckley was undergoing egg freezing, there was an initial delay, due to a cyst on one of her ovaries: “That was a bit of a blow, because it was meant to take six weeks and mine went on to three months.”
Despite this initial obstacle, she did not experience side effects from the medications or hormones.
The most challenging part was leading up to the egg collection: “Coming close to the date that they are due to be extracted, it’s extremely, extremely uncomfortable; you want to burst. It’s so full, because you normally wouldn’t have that many eggs.
“The medications are timed to the last minute, especially that last activating one that you need to take. You need to be prepared to be really, really regimental with your routine. Having people around you for support, as well. I felt OK until I got to those last 48 hours, where I couldn’t wait to go in and get [the eggs] out.”
The clinic Logan Buckley chose for her treatment had an online portal that was a real support to her: “You had access to support 24 hours a day, seven days a week. If there was anything at all you were slightly concerned about, you could pop it into the portal, and they would get back to you in lightning speed. That was really reassuring.”
At the age of 32, in 2003, Karen, from Dublin, embarked on her IVF journey. She had a 12-year-old child from a previous relationship. She subsequently met and married another man. He had fertility complications from a bout of the mumps he’d had as a teenager.
At the hospital fertility clinic Karen attended, she had a combination of frozen embryos and frozen eggs. She and her husband went on to have two children from two frozen embryos: A son, now 21, and a daughter, who has just turned 18.
Karen’s experience was overall “very positive”: “I was very well looked after. Both my embryos took first time; the doctor said I was in a 5% statistic of it working first time. The hardest part was having to do the injections before you have an egg collection and all of that process.”
Fertility treatment is a costly undertaking. Karen says: “The banter in my house is, ‘I have a receipt for you pair!’ It was a financial burden, but when you’re desperate, you’d beg, borrow, and steal. My mother-in-law gave us a good handout financially.”
The Government is now subsidising one cycle of IVF for qualifying couples. Egg freezing for fertility preservation is not included in this provision. Irish Life, Laya, and VHI include provisions for egg freezing in some of their plans, typically up to a cost of € 1,000.
Egg-freezing costs approximately €3,000 per cycle and approximately €300 per year for storage.
In Ireland, the storage period is unlimited until the age of 49.
While Irish fertility clinics operate to international standards, there is no regulatory authority or national clinical governance framework for the fertility services sector.
Lauren Murphy says the fertility sector has repeatedly called for regulation. In Britain, the regulator is the Human Fertilisation and Embryology Authority.
The necessity of regulatory oversight is apparent, and it becomes even more evident as demand for such services increases and new service providers enter the market.
Ipsos B&A designed and implemented a research project for the involving a nationally representative sample of n=1,078 women over the age of 16 years.
The study was undertaken online with fieldwork conducted between April 30 and May 15, 2025.
The sample was quota controlled by age, socio-economic class, region and area of residence to reflect the known profile of women in Ireland based on the census of population and industry agreed guidelines.
Ipsos B&A has strict quality control measures in place to ensure robust and reliable findings; results based on the full sample carry a margin of error of +/-2.8%.
In other words, if the research was repeated identically results would be expected to lie within this range on 19 occasions out of 20.
A variety of aspects were assessed in relation to women’s health including fertility, birth, menopause, mental health, health behaviour, and alcohol consumption.










