Prison and mental illness: Five myths and some solutions
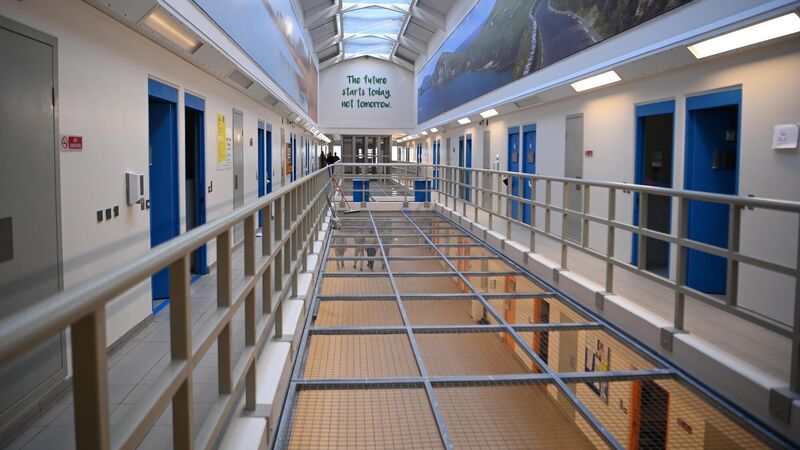
A prison is not a hospital. Prisons focus on security and order, which often conflict with medical priorities. File picture: Dan Linehan
- Gautam Gulati is adjunct professor at the School of Law, University College Cork.
- Brendan Kelly is professor of psychiatry at Trinity College Dublin





